
One of the most common and quickly spreading chronic illnesses in the world is diabetes. It is an illness that impacts the body’s ability to metabolize glucose, or blood sugar, which serves as the body’s cells’ primary energy source. Blood glucose levels that are too high or too low can cause a number of problems that impact different systems and organs. Diabetes can be classified into two primary types: Type 1 and Type 2 diabetes, with gestational diabetes and other forms also being notable. Understanding the causes, symptoms, management strategies, and potential complications of diabetes is essential to managing the disease and improving quality of life for those affected.
What is Diabetes?
The inability of the body to appropriately control blood sugar levels is known as diabetes. Through the food we eat, glucose, a necessary energy source, enters the body. In a healthy individual, the pancreas secretes the hormone insulin, which facilitates the transfer of glucose from the bloodstream into cells for energy. This mechanism is disrupted in diabetics, resulting in either hyperglycemia (excess blood glucose) or hypoglycemia (insufficient cell glucose).
Types of Diabetes
Although there are other forms of diabetes, Type 1 and Type 2 are the most prevalent. The causes, risk factors, and treatment approaches vary for each type.
1. Type 1 Diabetes
The immune system of the body targets and kills the insulin-producing cells of the pancreas in type 1 diabetes, sometimes referred to as insulin-dependent diabetes. Because of this, individuals with Type 1 diabetes need lifelong insulin therapy because they make little to no insulin. Although type 1 diabetes can occur at any age, it is usually identified in childhood or early adulthood.
Causes: Although the precise etiology of Type 1 diabetes is unknown, it is thought to be a combination of an immunological reaction and a hereditary susceptibility. The disease may begin as a result of environmental factors, including viral infections.
Symptoms: Symptoms of Type 1 diabetes include excessive thirst, frequent urination, exhaustion, hazy eyesight, unexplained weight loss, and sluggish healing of wounds.
Management: Type 1 diabetes is primarily treated with insulin therapy. Patients may need to utilize an insulin pump or administer insulin several times during the day. Insulin, food, exercise, and routine blood sugar monitoring are all essential components of blood sugar management.
- 2. Type 2 Diabetes
Type 2 diabetes is the most prevalent type of the disease, making up around 90% of all cases. In Type 2 diabetes, the body either stops producing enough insulin to maintain normal glucose levels or becomes resistant to it, which causes blood sugar levels to rise over time.
Causes: Although lifestyle factors including obesity, poor food, and lack of exercise are important contributors to type 2 diabetes, hereditary factors also play a role. Other factors include age, family history, and ethnicity (with Native American, Hispanic, and African American groups having higher prevalences).
Symptoms: Increased thirst, frequent urination, impaired vision, exhaustion, slow-healing wounds, and recurring infections are some of the symptoms of Type 2 diabetes that appear gradually.
Management: Adopting a balanced diet, increasing physical activity, and maintaining a healthy weight are some of the lifestyle modifications that are frequently used to control type 2 diabetes. Insulin therapy may be required in certain situations, and oral medicines, such as metformin, are frequently utilized. Maintaining a healthy lifestyle and routinely checking blood sugar levels are essential parts of controlling the condition.
- Gestational Diabetes
Pregnant women who have gestational diabetes are more likely to develop Type 2 diabetes later in life. Gestational diabetes is characterized by elevated blood sugar levels that develop during pregnancy and typically go away after childbirth, and it affects approximately 2-10% of pregnant women.
Causes: Gestational diabetes can result from hormonal changes during pregnancy that reduce the body’s sensitivity to insulin. Risk factors include age (over 25), obesity, and a family history of diabetes.
Symptoms: Since gestational diabetes usually shows no symptoms, screening examinations are crucial for expectant mothers. If symptoms do appear, they could include weariness, increased thirst, and frequent urination.
Management: A nutritious diet, consistent exercise, and blood sugar monitoring are all important components of managing gestational diabetes. Insulin injections could be necessary in certain situations. Blood sugar levels typically return to normal after giving delivery, but women with gestational diabetes should still be closely watched.
- Other Forms of Diabetes
Monogenic diabetes and steroid-induced diabetes are two less prevalent types of the disease that are brought on by genetic abnormalities or the use of particular drugs. These types are uncommon and call for customized treatment plans.
Risk Factors for Diabetes
Diabetes is more likely to develop in those who have certain characteristics. Although these risk factors varies for each type of diabetes, they often consist of the following:
- Genetics: Type 1 and Type 2 diabetes are more likely to occur in families with a history of the disease.
• Age: As people age, particularly after the age of 45, their chance of having Type 2 diabetes increases.
• Obesity: One of the main risk factors for Type 2 diabetes is excess body fat, particularly around the abdomen.
• Lack of Exercise: People who lead sedentary lives are more likely to develop Type 2 diabetes.
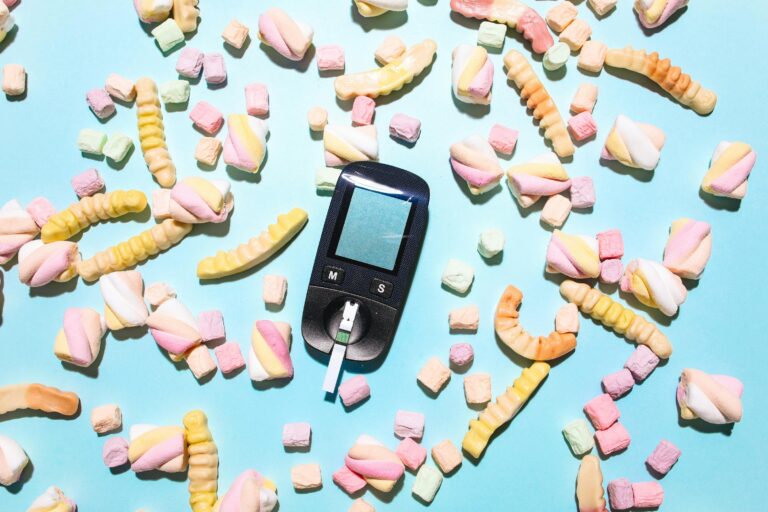
• Diet: Type 2 diabetes can develop as a result of a poor diet, especially one heavy in processed foods, sweets, and fats.
• Ethnicity: People of African American, Hispanic, Native American, and Asian American descent are more likely to develop diabetes than other ethnic groups.
Symptoms of Diabetes
The kind of diabetes and the health level of the individual both affect the symptoms. Both Type 1 and Type 2 diabetes frequently present with the following symptoms:
- Increased thirst and dry mouth
- Frequent urination
- Fatigue or feeling weak
- Blurred vision
- Unexplained weight loss (more common in Type 1)
- Slow healing of wounds or frequent infections
- Nausea and vomiting (in severe cases of high blood sugar)
- Numbness or tingling in hands or feet (in Type 2)
Type 2 diabetes frequently doesn’t manifest symptoms until complications arise. For individuals who are at risk, routine screening is crucial because of this.

Complications of Diabetes
Diabetes can cause major, potentially fatal consequences if it is not treated. Typical complications include the following:
- Cardiovascular Disease: Elevated blood sugar can harm blood arteries and raise the risk of high blood pressure, heart disease, and stroke.
2. Nerve Damage (Neuropathy): Long-term elevated blood sugar levels can harm nerves, resulting in tingling, discomfort, or loss of feeling in the limbs.
3. Kidney Damage (Nephropathy): Diabetes is a major contributor to kidney disease, which, if ignored, can lead to kidney failure.
4. Eye Damage (Retinopathy): Blindness may result from high blood sugar’s damaging effects on the retina’s blood vessels. - Foot Issues: Infections, ulcers, and even amputations can result from nerve damage and inadequate circulation in the feet.
6. Skin Infections: Because diabetes raises blood sugar levels, people with the disease are more vulnerable to bacterial and fungal infections.
7. Mental Health: Diabetes has been associated with a higher risk of anxiety, depression, and other mental health issues, which may have an impact on how well the disease is managed.
Diagnosis of Diabetes
Diabetes is diagnosed through blood tests, including:
- Blood glucose is measured using the Fasting Blood Sugar Test following an overnight fast. Diabetes is indicated by a fasting blood sugar level of 126 mg/dL or above.
2. After fasting and consuming a sweet solution, the oral glucose tolerance test (OGTT) measures blood glucose levels. After two hours, diabetes is indicated by a value of 200 mg/dL or above.
3. The hemoglobin A1c test calculates the mean blood sugar level throughout the previous two to three months. Diabetes is indicated by an A1c reading of 6.5% or greater.
Treatment and Management of Diabetes
Diabetes cannot be cured, but it can be effectively controlled with medicine, lifestyle modifications, and routine blood sugar checks. Preventing problems and maintaining blood sugar levels within a specific range are the objectives of treatment.
1. Lifestyle Modifications
- Healthy Diet: Blood sugar levels can be controlled with a balanced diet full of whole grains, veggies, lean meats, and healthy fats. Cutting back on processed foods and sugar is essential for managing Type 2 diabetes.
• Physical Activity: Frequent exercise lowers blood sugar levels and improves the body’s usage of insulin. Every week, try to get in at least 150 minutes of moderate-intensity exercise.
• Weight management: Keeping a healthy weight lowers the chance of problems and enhances insulin sensitivity.
• Blood Sugar Level Monitoring: Diabetes management requires routine blood sugar checks. This aids people in comprehending how their blood sugar levels are impacted by diet, activity, and medications.
2. Medications
- Type 1 Diabetes: In order to control blood sugar levels, individuals with Type 1 diabetes require insulin therapy. Insulin pumps or injections are two ways that insulin can be administered.
• Type 2 Diabetes: To assist control blood sugar levels, doctors may prescribe drugs such as Sulfonylureas, metformin, and SGLT2 inhibitors. In certain cases, insulin therapy may also be necessary.
- 3. Regular Check-Ups
To track the management of diabetes and identify any complications early, it’s critical to have regular check-ups with a healthcare professional.
Advancements in Diabetes Treatment and Technology
Significant advancements have been made in the management and treatment of diabetes in recent years. New drugs and advancements in medical technology have made it simpler for diabetics to control their disease and lower their risk of complications. Among the noteworthy developments are:
1. Continuous Glucose Monitors (CGMs)
The creation of continuous glucose monitoring devices (CGMs) is among the most significant developments in the treatment of diabetes. Without the necessity for fingerstick testing, CGMs enable people to continuously check their blood glucose levels day and night. This technology helps users make timely changes to their insulin dosages or lifestyle choices by giving them real-time feedback and alerting them when their blood sugar levels are too high or low.
CGMs have revolutionized the way persons with Type 1 diabetes regulate their blood sugar levels by providing a more thorough and practical approach. A “closed-loop” system is created when certain CGMs are connected with insulin pumps, which can automatically modify insulin dosage in response to real-time glucose readings.
2. Insulin Pumps
Insulin is continuously delivered throughout the day by tiny, electronic devices called insulin pumps. An insulin pump offers a consistent and regulated supply of insulin, in contrast to conventional insulin injections, which call for several daily doses. For those with Type 1 diabetes, this can improve overall management and help avoid blood glucose swings.
CGMs are frequently used in conjunction with modern insulin pumps to enable more accurate management and lessen the need for manual insulin changes. It has been demonstrated that insulin pumps enhance blood sugar regulation, lower the risk of hypoglycemia, and enhance quality of life.
3. Artificial Pancreas Systems
In order to build a closed-loop system that replicates the operation of a healthy pancreas, artificial pancreas systems integrate insulin pumps and CGMs. More accurate blood sugar control is made possible by these devices, which automatically modify insulin dosage in response to real-time glucose measurements. Artificial pancreas devices, which are still in the research and development stage, have the potential to significantly enhance the quality of life for people with Type 1 diabetes by lessening the strain of continuous insulin administration and monitoring.
4. Medications: GLP-1 Agonists and SGLT2 Inhibitors
Newer drugs like SGLT2 inhibitors (like empagliflozin) and GLP-1 receptor agonists (like liraglutide) have shown promise in the treatment of Type 2 diabetes. By increasing insulin sensitivity, decreasing the liver’s synthesis of glucose, and delaying digestion, these medications help to stabilize blood sugar levels.
Additionally, GLP-1 agonists aid in weight loss, which is advantageous for overweight or obese people with Type 2 diabetes. In addition to helping regulate blood sugar, SGLT2 inhibitors also lower blood pressure and lower the risk of cardiovascular disease, which is a common risk factor for diabetic complications.
5. Stem Cell Research and Potential Cures
As a possible treatment for Type 1 diabetes, researchers are also looking at stem cell therapies. The objective is to employ stem cells to repair the pancreatic beta cells that produce insulin, which are damaged in people with Type 1 diabetes. Even while this research is still in its infancy, it gives optimism that a Type 1 diabetes cure may one day be developed.
The Role of Lifestyle in Managing Diabetes
Effective diabetes management requires lifestyle decisions in addition to medication and technology. Blood sugar control and general health improvement can be greatly aided by a combination of a healthy diet, regular exercise, and stress reduction techniques.
1. Nutrition and Diabetes
Maintaining a healthy, balanced diet is essential for diabetics. Blood sugar levels can be controlled with a diet that prioritizes entire foods including fruits, vegetables, lean meats, whole grains, and healthy fats. The following are some crucial dietary tactics for diabetes management:
- Carbohydrate Counting: Knowing how to count carbohydrates may help people with diabetes, particularly those receiving insulin therapy. Based on their food intake, this aids them in estimating how much insulin they require.
• Low Glycemic Index (GI) Foods: Whole grains, legumes, and non-starchy vegetables are examples of foods with a low GI that raise blood sugar levels more slowly and are therefore better for diabetics.
• Portion Control: To prevent overindulging and maintain stable blood sugar levels, portion control is crucial. Consistent energy levels can be maintained by eating smaller, more frequent meals.
• Limit Processed Foods and Sugars: The key to treating diabetes is consuming fewer processed foods, sugary snacks, and sugary drinks. Blood glucose levels can rise quickly after eating certain items.
2. Physical Activity
One of the best strategies for improving insulin sensitivity and managing Type 2 diabetes is exercise. Frequent exercise lowers blood sugar, maintains a healthy weight, and improves the body’s ability to use insulin. Among the main advantages of exercise for diabetes are:
- Increased Insulin Sensitivity: Exercise improves the body’s cells’ ability to react to insulin, which lowers the requirement for larger insulin dosages.
• Weight management: Losing or maintaining weight through regular exercise can improve blood sugar regulation and reduce the risk of Type 2 diabetes.
• Lower Risk of Heart Disease: Individuals who have diabetes are more likely to develop cardiovascular disease. Frequent exercise lowers blood pressure, cholesterol, and inflammation, all of which contribute to better heart health.
• Enhanced Mood and Energy: Exercise improves mood and energy levels while lowering stress, both of which can benefit general mental and physical health.
People with diabetes should strive for at least 150 minutes of moderate-intensity activity per week, such as brisk walking or cycling, according to the American Diabetes Association (ADA).
3. Stress Management
Blood sugar levels might be adversely affected by ongoing stress. Stress causes the body to create cortisol and other hormones that might raise blood sugar levels. Controlling stress is a key component of diabetes management for those who have the condition.
In addition to reducing stress through methods like yoga, meditation, deep breathing, and mindfulness exercises, managing general well-being requires scheduling leisure time, hobbies, and social interactions.
Diabetes and its Economic and Social Impact
Diabetes has a major impact on society and the economy in addition to an individual’s health. The International Diabetes Federation (IDF) estimates that the global economic cost of diabetes was over $1 trillion in 2019. This figure is projected to climb as the disease’s prevalence rises.
1. Healthcare Costs
Significant medical costs are associated with managing diabetes, including prescription drugs, monitoring equipment, doctor visits, and complications treatment. Healthcare systems may be severely impacted by the expenses of treating diabetes, particularly in nations with aging populations and rising obesity rates.
For instance, those with diabetes in the US spend almost 2.3 times as much on healthcare as those without the condition. In order to lessen long-term financial strain, prevention, early detection, and efficient management are crucial given the high expenses of diabetes care.
2. Impact on Quality of Life
Additionally, diabetes can significantly affect a person’s quality of life. It might take a lot of time and mental energy to take medications, maintain a tight diet, and control blood sugar levels. Physical restrictions and a diminished sense of wellbeing might also result from the possibility of consequences like neuropathy, visual issues, and amputations.
Stress, anxiety, and depression are among the mental health conditions that can be exacerbated by the emotional toll of having diabetes. Diabetes patients frequently have to follow treatment regimens and undergo close monitoring for the rest of their lives, which can be emotionally and psychologically taxing.
3. Workforce Productivity
Workplace productivity might also be impacted by diabetes. Absenteeism, reduced productivity at work, and a higher chance of disability or early retirement due to comorbidities are all consequences of the disease. Employees with diabetes may require adjustments from their employers, such as flexible work schedules or time off for doctor’s appointments.
The Path Forward: Prevention and Education
Diabetes management and prevention call for teamwork. Reducing the rising prevalence of diabetes requires public health measures that emphasize early identification, healthy lifestyles, and awareness-raising.
- Prevention Programs: Weight control, regular exercise, and a nutritious diet are all part of the effort to lower the prevalence of Type 2 diabetes. People can lower their risk of acquiring diabetes and adopt healthier lives with the support of community-based initiatives, school programs, and public health campaigns.
2. Education and Awareness: To guarantee early diagnosis and treatment, it is essential to increase knowledge of the warning signs, symptoms, and risk factors of diabetes. Early detection of diabetes and the avoidance of complications can be achieved by educating people about the value of routine tests, especially for those who are more susceptible. - Access to Healthcare: It’s critical to guarantee that people have access to reasonably priced medical care and diabetes management resources, such as insulin, glucose monitors, and prescription drugs. Globally, efforts to ensure that everyone has access to diabetes care can help people avoid complications and achieve better results.
(FAQs) about diabetes:
1. What are the main differences between Type 1 and Type 2 diabetes?
- Type 1 diabetes is an autoimmune disease in which the pancreatic cells that produce insulin are attacked and destroyed by the immune system. Insulin must be taken everyday for the rest of one’s life if one has Type 1 diabetes.
• Insulin resistance or insufficient insulin production are the two main causes of type 2 diabetes. Although it is more prevalent in adults, lifestyle factors like poor diet and inactivity are also contributing to an increase in its diagnosis in children and adolescents. Usually, oral medicines, lifestyle modifications, and occasionally insulin are used to treat type 2 diabetes.
2. What are the common symptoms of diabetes?
Increased thirst and frequent urination, fatigue or weakness, and unexplained weight loss (particularly in Type 1) are common signs of both Type 1 and Type 2 diabetes.
- Slow wound or cut healing; blurred eyesight;
- Hand or foot numbness or tingling (particularly prevalent in Type 2)
It’s crucial to remember that Type 2 diabetes can progress slowly and that some people may not exhibit any symptoms until problems start to show.
3. Can diabetes be prevented?
Yes, altering one’s lifestyle can frequently prevent or postpone Type 2 diabetes. A balanced diet that includes whole grains, veggies, and healthy fats is one of the most important preventive strategies.
- Maintaining a healthy weight
• Getting regular exercise (at least 150 minutes of moderate activity each week)
• Controlling stress levels; - Steering clear of tobacco and heavy alcohol use
Although there is no way to prevent Type 1 diabetes, complications can be avoided with early detection and appropriate management.
4. How is diabetes diagnosed?
A number of tests can be used to detect diabetes:
- Fasting Blood Sugar Test: Diabetes is indicated by a blood sugar level of 126 mg/dL or above following a fast.
• Oral Glucose Tolerance Test (OGTT): Diabetes is diagnosed if, following consumption of a sweet solution, blood sugar levels reach 200 mg/dL or above.
• Hemoglobin A1c Test: Diabetes is indicated by a value of 6.5% or more. The average blood
sugar levels over the previous two to three months are measured by this test.
The right test will be suggested by a healthcare professional depending on each patient’s unique situation and risk factors.
5. What are the long-term complications of diabetes?
Diabetes can cause major complications if it is not controlled, such as:
- Cardiovascular Disease: A higher chance of high blood pressure, heart disease, and stroke.
• Neuropathy (nerve damage): May result in tingling, discomfort, or loss of feeling in the hands and feet.
• Nephropathy, or kidney damage, can result in renal failure.
• Retinopathy: Damage to the retina’s blood vessels increases the chance of blindness.
• Foot Issues: Infections or even amputations may result from poor circulation and nerve damage.